How is a breast biopsy done?
Fine-needle aspiration biopsy
A fine-needle aspiration biopsy may be done by an internist, family medicine doctor, radiologist, or a general surgeon. The biopsy may be done in your doctor's office, a clinic, or the hospital.
You will take off your clothing above the waist. A paper or cloth gown will cover your shoulders. The biopsy will be done while you sit or lie on an examination table. Your hands may be at your sides or raised above your head (depending on which position makes it easiest to find the lump).
Your doctor numbs your skin with a shot of numbing medicine where the biopsy needle will be inserted. Once the area is numb, a needle is put through your skin into your breast tissue. Ultrasound may be used to guide the placement of the needle during the biopsy. If the lump is a cyst, the needle will take out fluid. If the lump is solid, the needle will take a sample of tissue. The biopsy sample is sent to a lab to be looked at under a microscope. You must lie still while the biopsy is done.
The needle is then removed. Pressure is put on the needle site to stop any bleeding. A bandage is put on. A fine-needle aspiration biopsy takes about 5 to 15 minutes.
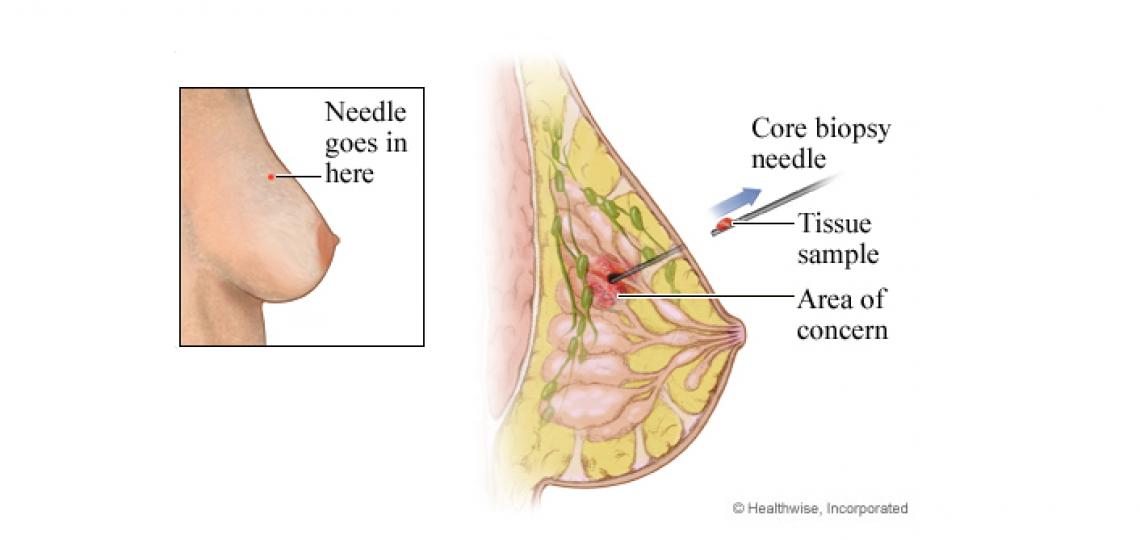
Core needle biopsy
A core needle biopsy may be done by an internist, family medicine doctor, radiologist, or general surgeon. The biopsy may be done in your doctor's office, a clinic, or the hospital.
You will take off your clothing above the waist. A paper or cloth gown will cover your shoulders. The biopsy will be done while you sit or lie on an examination table. Your hands may be at your sides or raised above your head (depending on which position makes it easiest to find the lump).
Your doctor numbs your skin with a shot of numbing medicine where the biopsy needle will be inserted. Once the area is numb, a small cut is made in your skin. A needle with a special tip is put into the breast tissue. The doctor will take 3 to 12 samples to get the most accurate results.
The needle is removed. Pressure is put on the needle site to stop any bleeding. A bandage is put on. This may be repeated several times to make sure enough tissue samples were collected.
A core needle biopsy takes about 15 minutes.
Stereotactic biopsy
A stereotactic biopsy is done by a radiologist. The biopsy is done in a radiology department.
You will take off your clothing above the waist. A paper or cloth gown will cover your shoulders. You may sit in a chair, or you may lie on your stomach on a special table that has a hole for your breast to hang through. A mammogram or MRI is used to find the exact site for the biopsy.
Your doctor numbs your skin with a shot of numbing medicine where the biopsy needle will be inserted. Once the area is numb, a small cut is made in the skin. With a special X-ray to guide the needle, it is put into the suspicious area. Usually, more than one sample is taken through the same cut. You will need to be very still while the biopsy is done.
The small cut made for the needle does not usually need stitches. Pressure is put on the needle site to stop any bleeding. A bandage is put on. A small metal marker (clip) is usually placed in the area where the biopsy sample was taken. This is done to locate the exact spot where the tissue sample was taken.
The metal marker will stay in your breast if you do not have cancer. You will not be able to feel it, and it will not set off metal detectors. You can still have an MRI safely. When you have mammograms in the future, the radiologist will be able to see the metal marker.
This type of breast biopsy takes about 60 minutes. But most of this time is needed for the mammogram or MRI and finding the area for the biopsy.
Vacuum-assisted biopsy
A vacuum-assisted biopsy is done by a radiologist or a surgeon. This method may be used for a core needle biopsy or a stereotactic biopsy. The biopsy may be done while you sit or lie on an examination table. Or you will lie on your stomach on a special table that has an opening for your breast. A mammogram, ultrasound, or MRI is used to find the exact site for the biopsy.
Your doctor numbs your breast with a shot of local anesthetic. Once the area is numb, a small cut is made in your skin. A hollow probe with a special tip is put into the breast. Tissue is gently vacuumed into the probe. With this type of biopsy, the doctor can take more than one sample without removing the probe.
After the probe is removed, pressure is put on the site to stop any bleeding. The small cut does not need stitches and leaves only a small scar.
A vacuum-assisted core biopsy takes less than an hour.
Open biopsy
An open biopsy is done by a general surgeon, gynecologist, or family medicine doctor. The biopsy may be done in a surgery clinic or the hospital.
You will need to take off all or most of your clothes above the waist. You will be given a gown to use during the biopsy. The biopsy will be done while you sit or lie on an examination table. Your hands may be at your sides or raised above your head (depending on which position makes it easiest to find the lump).
An open biopsy can be done using local or general anesthesia. If local anesthesia is used, you may also be given a sedative.
If you have general anesthesia, an intravenous (IV) line will be put in your arm to give you medication. You will not be awake during the biopsy.
After the breast is numb (or you are unconscious), your doctor makes a cut through the skin and into the breast tissue to the lump. If a small wire was placed using mammogram to mark the biopsy site, your doctor will take a biopsy from the area at the tip of the wire.
Stitches are used to close the skin, and a bandage is put on. You will be taken to a recovery room until you are fully awake. You can usually return to your normal activities the next day.
An open biopsy takes about 60 minutes.
Information About Your Tumor
After you have a biopsy, the pathologist sends a report describing the features of your tumor to your doctor. This includes the results of special tests performed on the tumor tissue that are important in determining which treatment will be best for you.
The two most informative factors in determining your treatment are the tumor size and the extent of lymph node involvement. Other helpful information is tumor grade, hormone receptor status, ploidy and S-phase.
Tumor size. Noted in centimeters.
Lymph node involvement. A tumor that grows into the blood vessels or lymph nodes is considered more likely to spread. The pathologist will count the number of lymph nodes that have breast cancer cells in them.
Tumor grade. The grade of the tumor is determined by how abnormal the cancer cells appear when examined under a microscope. Cells that are more normal appearing, Grade I, tend to be less aggressive. Cells that are the least normal appearing, Grade III, are more aggressive.
Estrogen receptor (ER) and Progesterone receptor (PR). Proteins found in some breast cancer cells to which estrogen and progesterone will attach. A special test measures the amount of these proteins in breast cancer tissue. Breast cancer cells that are estrogen receptor positive (ER+) are more likely to need the estrogen to grow. Breast cancer cells that are progesterone positive (PR+) also are more likely to need estrogen to grow. Breast cancer that is ER or PR positive usually responds to hormonal estrogen treatment, like tamoxifen.
Ploidy and S-phase (proliferative fraction). Special technique used to tell whether abnormal amounts of DNA are present in the cancer cells (aneuploidy) and how many cells are dividing at any point in time ( percent S-phase). These characteristics can sometimes be used to estimate the aggressiveness of the tumor.
HER2/neu. Gene that makes Human Epidermal growth factor Receptor 2. The protein produced is HER2/neu. In normal breast tissue cells, the HER2 gene produces a protein that is found on the cell surface. This protein is thought to play a role in normal cell growth by signaling the cell to divide and multiply. Cancerous breast tissue cells that have abnormally high amounts of HER2 can sometimes divide at a faster rate. About 20 percent of women with breast cancer have abnormally high HER2 amounts. This marker can be helpful in determining whether Herceptin is a treatment option for a woman with breast cancer.
Tumor markers. Tumor cells sometimes produce "markers." Tumor markers are substances sometimes found in increased amounts in blood or in the presence of breast cancer. Tumor markers that are sometimes used in the management of breast cancer include the CEA and CA 27-29.
In some situations, they can be useful, in addition to other means, for assessing response to treatment. They have not been shown to be useful in detecting if a cancer has come back or in detection of early breast cancer.
© 2016-2019 Healthwise, Incorporated.








 Credit
Credit