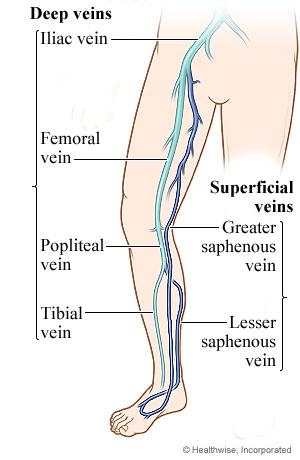
Deep vein thrombosis (DVT) is a blood clot (thrombus) in a deep vein, usually in the legs. These clots require medical care right away.
These clots are dangerous because they can break loose, travel through the bloodstream to the lungs, and block blood flow in the lungs (pulmonary embolism). Pulmonary embolism is often life-threatening. DVT can also lead to long-lasting problems. It may damage the vein and cause the leg to ache, swell, and change color.
Clots can also form in superficial veins. Blood clots with inflammation in superficial veins (called superficial thrombophlebitis or phlebitis) rarely cause serious problems.
Blood clots most often form in the calf and thigh veins, and less often in the arm veins or pelvic veins. Diagnosis and treatment of DVT in other parts of the body are similar.
What causes deep vein thrombosis (DVT)?
Causes of a blood clot in a deep vein (DVT) include:
- Slowed blood flow. This can happen when you're not active for long periods of time. For example, clots can form if you are paralyzed, are confined to bed, or must sit while on a long flight or car trip.
- Abnormal clotting problems that make the blood clot too easily or too quickly. For example, some people have blood that clots too easily, a problem that may run in families.
- Surgery or an injury to the blood vessels. Blood is more likely to clot in veins shortly after they are injured.
- Cancer.
What are the symptoms of deep vein thrombosis (DVT)?
Deep vein thrombosis often doesn't cause symptoms. Or it may cause only minor ones. When symptoms happen, they include:
- Swelling in the affected area.
- Redness and warmth in the affected area.
- Pain or tenderness. You may have pain only when you touch the affected area or when you stand or walk.
- Sometimes a pulmonary embolism is the first sign that you have DVT.
If your doctor thinks you may have DVT, you will probably have an ultrasound test. You may have other tests as well.
How is deep vein thrombosis (DVT) treated?
The main goals of treatment for DVT are:
- To prevent the blood clot from getting larger.
- To prevent the blood clot from traveling to the lungs (pulmonary embolism).
- To prevent post-thrombotic syndrome. This is a condition that can cause pain, sores, and swelling of the affected leg.
- To prevent blood clots from coming back.
- Treatment includes medicine and self-care.
Medicine
DVT is usually treated with anticoagulant medicines. These medicines are often called blood thinners, but they don't actually thin the blood. They prevent blood clots by increasing the time it takes a blood clot to form. They also help prevent existing blood clots from becoming larger.
You might take anticoagulants for at least 3 months. The length of time will vary based on your own health, where the blood clot is in your leg, and your risk for a pulmonary embolism.
Other treatments may be used in the hospital for some people. These treatments include thrombolytic medicine and vena cava filters. But these treatments aren't common. They might be used for people who are at risk for serious problems from DVT.
Self-care
Your doctor may also recommend self-care to relieve symptoms. This care includes:
- Walking.
- Propping up (elevating) your leg.
- Wearing compression stockings.








 Credit
Credit