About the Program
Next opening: 2027-2028
Number of positions: 1
Length: 1 year
This ACGME-accredited fellowship provides robust training in disorders of the luminal GI tract, pancreas and hepatic pathology (medical liver including liver transplantation), preparing trainees for a career in an academic or private practice setting. Five GI pathologists provide clinical service, contribute to the research program of the GI section, and support the GI Pathology training program across four distinct hospital and outpatient settings.
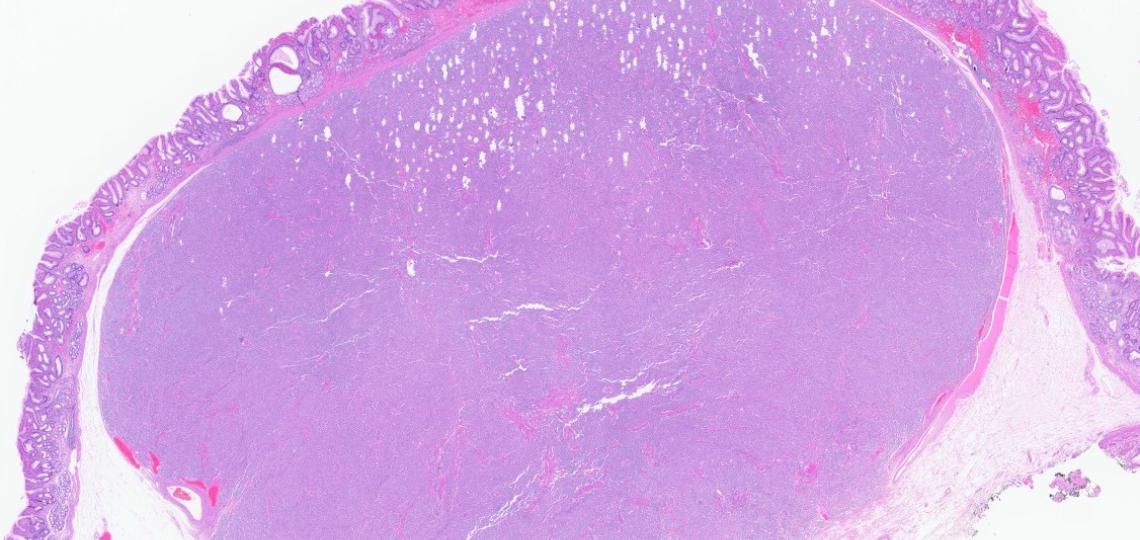
The GI pathology fellow will get exposure to a comprehensive spectrum of gastrointestinal surgical specimens, ranging from small biopsies to complex procedures, as well as hepatobiliary specimens. Training also includes reviewing consult digital slides from community practices in Texas. The fellow will have graduated responsibility in performing operating room consultations (frozen sections and gross examination). The fellow is expected to closely interact with surgeons/clinicians and pathology colleagues from community practice, actively participate in tumor boards, IBD/liver conferences, participate in research projects and will have the opportunity to attend and contribute to numerous didactic and clinical conferences.
Rotations
The fellow will rotate across two institutions: Baylor St. Luke’s Medical Center and Texas Children’s Hospital, with a one-month rotation at MD Anderson Cancer Center. Program strengths include extensive experience in routine and complex gastrointestinal pathology, pancreatic pathology, medical liver biopsies, liver transplantation, and pediatric pathology.
A one-week rotation in clinical gastroenterology is included, during which the fellow may observe advanced endoscopic procedures such as EMR/ESD and EUS-guided FNA/FNB performed by experienced gastroenterologists.
Stipends and Benefits
Visit the Graduate School of Biomedical Sciences page on stipends and benefits for fellows.








