About STaR
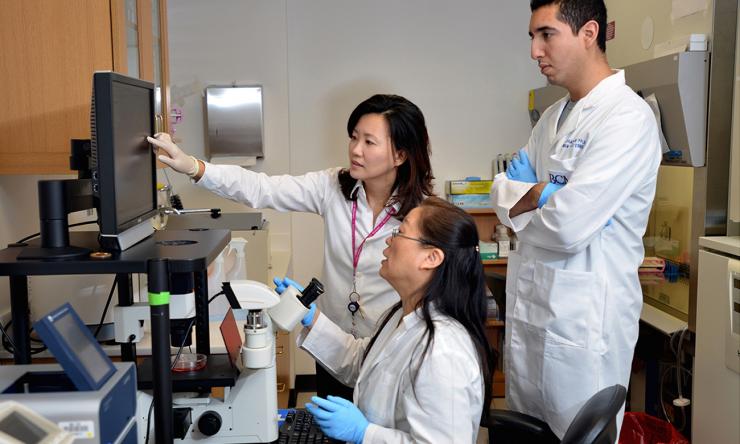
The Stem Cells and Regenerative Medicine Center (STaR) was founded in 2005 to facilitate stem cell research of all types at Baylor College of Medicine, and the clinical translation of such research into regenerative medicine.
Adult and embryonic stem cells have enormous therapeutic potential. Despite the great promise of stem cells, most therapeutic applications are years away, in part because many fundamental questions have yet to be answered.
The STaR Center's 30 associated investigator study adult and embryonic stem cells, as well as the role of cancer stem cells in contributing to relapse. We are interested in fundamental questions, such as understanding how stem cells are stimulated to regenerate tissues, and also practical issues, such as how to use stem cells to repair a patient's damaged tissue.
Research
In our center we study adult, embryonic, and cancer stem cells. The summaries below explain the work done by the core labs of the STaR Center.
Blair Benham-Pyle, Ph.D. studies molecular and cellular mechanisms regulating stem cell immortality and tissue regeneration. The lab combines high-throughput RNAi screens, genomics, and RNA FISH with the remarkable biology of regenerative planarian flatworms to discovery how cell types across an organism can coordinate stem cell proliferation and tissue regeneration while inhibiting aging and tumor initiation.
Andre Catic, M.D., Ph.D. joined the Stem Cells and Regenerative Medicine Center and the Huffington Center on Aging at Baylor College of Medicine in 2014 as a CPRIT Scholar in Cancer Research. His laboratory investigates how protein stability impacts gene regulation and cellular metabolism. The goal of this research is to understand, and eventually control, molecular mechanisms that are critical for aging and cancer.
Benjamin Deneen, Ph.D. seeks to unlock the enigmatic biology surrounding glial cell development and function in the brain. His work has revealed new paradigms for neural development and brain tumor growth, opening the door for innovative therapeutic interventions. His lab has built an interdisciplinary research program that draws on paradigms from development, disease, physiology, and genomics to better understand the nature of glial cells in the brain.
Bruno Di Stefano, Ph.D. joined the Stem Cells and Regenerative Medicine Center and the Center for Cell and Gene Therapy at Baylor College of Medicine in 2020 as a CPRIT Scholar. His current research aims to understand the post-transcriptional and epigenetic mechanisms that govern stem cell potency and cell fate decisions. The ultimate goal is to utilize these mechanistic insights for the development of new strategies to treat cancer and other complex diseases.
Margaret Goodell, Ph.D. is focused on understanding the mechanisms of regulation of normal and malignant hematopoiesis. Over the past 23 years, she has made innovative contributions in hematopoietic stem cell (HSC) biology, stem cell aging, epigenetic regulation of stem cells and the development of CRISPR tools for editing the genome of HSCs and for modulating DNA methylation.
Katherine King, M.D., Ph.D. began her own laboratory at Baylor College of Medicine after completing her residency, internship and fellowship here. The King Lab uses animal models of infection to investigate the effects of infection and inflammation on hematopoietic stem cell (HSC) biology. Research in the King Lab has implications for prevention and treatment of blood disorders related to inflammatory conditions, responses to infectious diseases, and competition between hematopoietic stem cell clones.
Daisuke Nakada, Ph.D. studies the molecular and cellular mechanisms that regulate self-renewal and differentiation in HSCs and leukemia. The lab uses mouse genetics, genome-editing tools, and epigenome profiling to understand how physiological changes and stress conditions stimulate HSCs, as well as how the mechanisms that regulate HSCs go awry to cause leukemia.
Ron Parchem, Ph.D. focuses on the mechanisms controlling stem cells in development and disease. This work is being applied to gain insight into a broad range of conditions, including common birth defects and brain cancer. For his research on cancer stem cells, Dr. Parchem has recently received funding from the Cancer Prevention and Research Institute of Texas (CPRIT), the V Foundation for Cancer Research and the Andrew McDonough B+ Foundation. He was recently recognized with an award from the Center for Cell and Gene Therapy for excellence in teaching.
Rachel Rau, M.D. has expertise in the biology of hematologic malignancies with a current focus on the genomic and epigenetics of leukemogenesis and chemoresistance. Her lab’s recent work includes a translational study defining the histone modifier, DOT1L as a novel epigenetic target for the treatment of AML with mutations of the gene DNMT3A and a mapping of the mutational landscape of mixed phenotype acute leukemia.
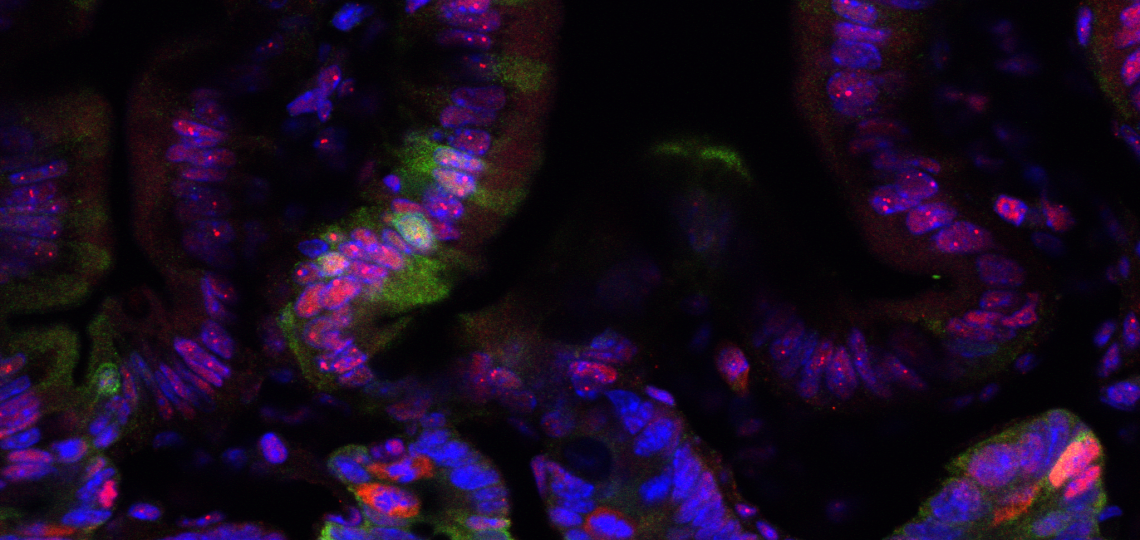
Noah Freeman Shroyer, Ph.D. is focused on understanding the mechanisms that control intestinal development and homeostasis, and translating this knowledge into novel therapeutic approaches to treat diseases of the intestine such as IBD and colorectal cancer. In addition to mechanistic studies, his lab developed novel organ culture methods to direct differentiation of human pluripotent stem cells into intestinal tissue to study intestinal development and disease, and has used intestinal stem cell-derived organoids in quantitative assays to evaluate intestinal stem cell activity.
Education
Graduate students from several departments and interdisciplinary training programs in which our faculty are members train at STaR. More details can be found in the Graduate School brochure.
Postdoctoral Training
Center Director Dr. Goodell holds an NIH NIDDK-funded T32 in Hematology, and trainees are also eligible for spots on Dr. Helen Heslop's NCI-funded Cell and Gene Therapy T32 training grant, as well as many other funding and fellowship opportunities. There are usually positions available in many laboratories. Contact the investigators directly for more information.
Human Stem Cell Core
The Human Stem Cell Core provides a wide range of products and services related to human pluripotent stem cell research, as well as hands-on training classes for basic and advanced stem cell culture techniques.
Center Director
Dr. Margaret Goodell is the director for the STaR Center.
As Seen in Cell Stem Cell
From the Labs blog discusses the Goodell Lab's finding that mutant PPM1D gives stem cells a survival advantage
Interviewed by Nature
Dr. Benjamin Deneen spoke to Nature about astrocyte diversity.









 Credit
Credit
