The Agent
Ebola Virus Disease
Ebola viruses cause a severe and often deadly illness known as Ebola virus disease (EVD; previously referred to as Ebola hemorrhagic fever). Fatality rates during EVD outbreaks can be as high as 90 percent. Ebola viruses produce hemorrhagic fever, a condition that also can be brought about by other types of viruses but Ebola produces one of the most lethal forms. In addition to the other symptoms of hemorrhagic fever – fever, headache, muscle pain, weakness, vomiting, and diarrhea – the more severe cases can include damage to blood vessels and extensive internal and external bleeding (hemorrhage). Mortality rates for EVD range from 25 percent to 90 percent, with an average of 50 percent. Death usually occurs as a result of shock due to fluid loss rather than blood loss.
There are no approved drugs or vaccines available to treat EVD, although experimental vaccines and therapeutics are being tested. Recovery seems to depend in part on how much virus a person was initially exposed to, how early treatment is started, and on the patient's age and immune response. Chances of survival can be improved with early supportive care including maintaining body fluids and electrolytes and monitoring blood pressure, which may allow enough time for the body's immune system to fight off the virus. Younger people appear to have better recovery rates than older people. Those who recover develop antibodies that may last at least 10 years. Some survivors develop long-term complications, such as joint and vision problems.
Ebola Virus Classification
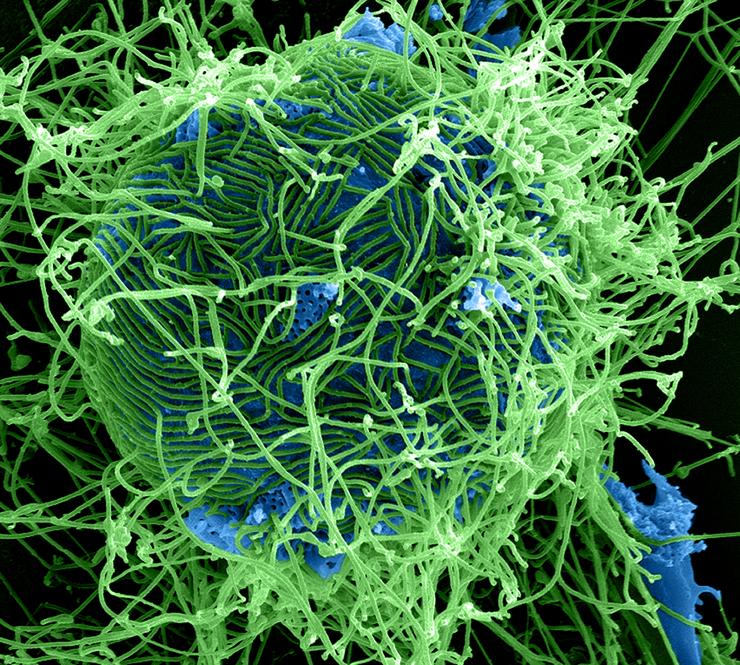
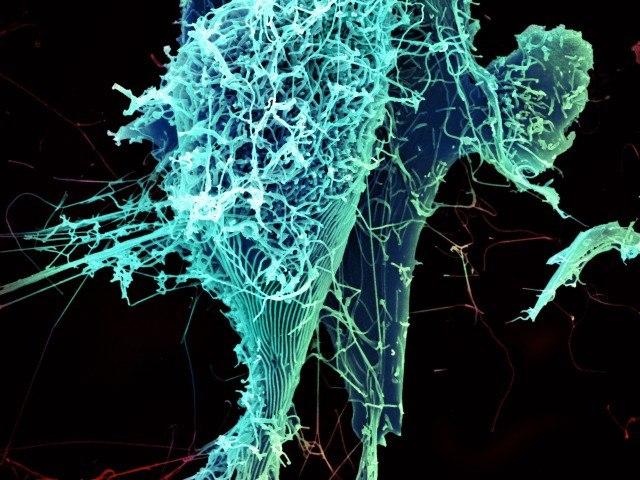
Ebola viruses belong to a family of viruses termed Filoviridae. Filovirus particles form long, sometimes branched, filaments of varying shapes, as well as shorter filaments, and may measure up to 14,000 nanometers in length with a diameter of 80 nanometers. Viral particles contain one molecule of single-stranded negative-sense RNA, enveloped in a lipid (fatty) membrane. New viral particles bud from the surface of their host cell. Although Ebola virus was only discovered in 1976, it is an ancient virus and is thought to have split from other viruses thousands of years ago.
There are five subtypes of Ebola viruses: Zaire, Sudan, Bundibugyo, Tai Forest (formerly known as Côte d’Ivoire), and Reston, each named after the location in which it was first identified. The first three subtypes have been associated with large EVD outbreaks in Africa. The Reston subtype is found in the Western Pacific and although it is highly pathogenic in nonhuman primates, it is not known to cause illness in humans. In addition to Ebola virus, there is one other member of the Filovirus family, known as Marburg virus (named after the city in Germany in which it was first discovered), that also causes hemorrhagic fever.
Spread of Ebola Virus
Ebola virus is spread through direct contact with blood or other bodily fluids, such as semen, feces, or vomit, of infected persons (or animals), including close contact with deceased EVD victims, which are highly infectious. Infection can also be spread through objects like needles and syringes or clothing and bedding that have been contaminated with the virus. Most cases of Ebola virus transmission occur between family members or in health care settings with inadequate infection control, because in these circumstances people are at highest risk of coming in contact with infected bodily fluids. The virus enters the body through a break in the skin or through the eyes, nose, or mouth of an unprotected person.
Unlike some other viruses, such as influenza or SARS, Ebola virus is not spread through the air. It is not spread by water or through mosquitoes or other insects. Ebola can be spread from person to person only while the infected person is displaying symptoms (although it has recently been recognized that the virus can persist in the semen of a small percentage of male survivors for more than a year). An infected person generally does not produce high levels of the virus when they first start to exhibit symptoms so the risk of transmission is low at this stage, but as the disease progresses and the amount of virus in the body increases, a person becomes more contagious. The incubation period ranges from 2 to 21 days, with an average of 8 to 10 days.
Ebola Virus Reservoir
Where does Ebola virus come from and where does it go between outbreaks? As with other viruses, the survival of Ebola depends upon a host organism(s). Humans are not the host organism - or natural reservoir - of Ebola viruses. Humans become infected when they come into contact with an infected host, although once humans become infected they can transmit Ebola to other people. The identification of the natural reservoir of a virus is of great interest to scientists, because this knowledge gives information as to the geographic range and ecological areas where humans may come in contact with animals or insects that may be the source of the disease.
The natural reservoir of Ebola appears to be the fruit bat. Researchers found evidence that three species of captured fruit bats showed evidence of symptomless infection – that is the bats had Ebola-specific genetic sequences in their bodies or evidence of an immune response to Ebola even though they did not exhibit signs of the disease. Fruit bats live in regions of Africa that include areas where Ebola outbreaks have occurred and are eaten by people in central Africa and may play a key role in transmitting Ebola to great apes and humans. Bats have been implicated as a reservoir of other viruses that cause deadly diseases including SARS and Marburg.
Infected bats can transmit the virus to monkeys and apes, so humans can become infected while killing or butchering these animals. Cooking destroys the virus, so the risk from infection comes from the preparation of bat or ape meat, not in eating cooked meat. Humans and animals may also become infected through contact with infected bats or fruit contaminated by infected bat droppings. However, the vast majority of people contract the virus through direct exposure to the body fluids of an infected person.
Ebola Outbreaks
Early Outbreaks
Ebola is considered an emerging infectious disease. It was first recognized in 1976 as the cause of twin outbreaks of disease near the Ebola River in the Democratic Republic of the Congo (then known as Zaire) and in a region of Sudan. Some 300 people in each country became infected. The mortality rate was 88 percent in Zaire and 53 percent in Sudan (the Zaire subtype is the most deadly). Although the circumstances of the original human infections are not known, the disease spread through close direct contact and as a result of unsafe and unsanitary hospital practices, such as the use of contaminated needles and the lack of sufficient containment measures.
Sporadic and smaller outbreaks have erupted over the succeeding years in the Democratic Republic of the Congo, Gabon, Uganda, and Sudan. An outbreak in the DRC in late August of 2014, that lasted several months, resulted in 66 cases and 49 deaths. As in prior outbreaks, the initial case was traced to the handling of infected bushmeat. This outbreak in the DRC was caused by a different variant of the Ebola virus that produced the much larger and wide-spread outbreak in the same year in West Africa.
The Reston Ebola Virus Outbreak
The Reston subtype of Ebola virus was first identified in 1989 in the United States in monkeys housed in a quarantine facility in Reston, Virginia. At least four humans became infected, but none became ill. Additional outbreaks of the Reston subtype occurred between 1989 and 1996 in Texas, Pennsylvania, and Italy. No humans suffered illness in any of these cases. The source of all the Reston subtype outbreaks was traced to a single facility in the Philippines that exported the monkeys. In July of 2009, the discovery of the Reston subtype in domestic pigs in the Philippines was reported. Genetic analysis suggests that the virus has been widely circulating in swine for many years, possibly even before the 1989 outbreak in the United States. The virus has been detected in farmers who have had contact with infected pigs, but they have not shown any signs of illness.
The 2014 Outbreak
In 2014, a large and rapidly spreading outbreak of EVD erupted, for the first time, in West Africa. Although it took several months for the disease to become recognized as Ebola, it appears that the first victim was a 2-year old boy in a small village in southeastern Guinea who died in December of 2013, followed by the deaths of several members of his family. Although these family members were not tested, their symptoms and the subsequent pattern of virus spread are consistent with the EVD outbreak. The child is thought to have played in a tree that housed Ebola-infected bats, so that he likely came in direct contact with the bats or their droppings. The virus transmitted by these bats is closely related to the Zaire Ebola virus.
In mid-March of 2014, cases of EVD in Guinea were recognized and reported to the World Health Organization and soon thereafter cases were reported in Liberia and then Sierra Leone. Reports came from multiple regions within these countries. Ebola arrived in Nigeria during July when a person who had had contact with an Ebola victim in Liberia traveled by plane to Nigeria and infected several contacts. In late August, Ebola reached a fifth country when Senegal confirmed its first and, to date, only case. Mali reported its first case in October after a symptomatic young girl traveled from Guinea to Mali and died shortly afterwards, and then an independent small cluster arose a short time later after an elderly man with undiagnosed disease traveled from Guinea to Mali. The outbreak was quickly contained in Mali, Senegal and Nigeria, but widespread transmission occurred in Liberia, Guinea, and Sierra Leone.
The initial transmission of Ebola virus outside of West Africa came to light in early October 2014 when a nursing assistant at a hospital in Spain contracted EVD after she had helped care for a missionary who had become infected in Sierra Leone and then flown to Spain. She recovered from EVD, and tests were negative for the presence of the virus following her illness. Several other people who contracted Ebola in West Africa were treated in hospitals in the United States and in Spain, Germany, the United Kingdom, France, and Norway, but to date no further transmission has occurred.
The first diagnosis of Ebola virus infection in the United States was announced on Sept. 30, 2014. Prior to traveling to Dallas, Texas, a man had had direct contact with a woman in Liberia who was dying of Ebola. His symptoms appeared only after he arrived in the United States. While seeking medical attention at a hospital in Dallas, his illness was not immediately recognized as Ebola and he was sent home. He was admitted to the same hospital three days later when his condition worsened, and he died ten days after he was admitted.
A nurse who had contact with this patient during his second hospital stay was confirmed to have EVD on Oct. 12. This was the first known case of transmission within the United States. A second nurse at the same hospital tested positive for Ebola three days later. Both nurses recovered and have been declared free of the virus. Other contacts of the Liberian patient, including family members who shared an apartment with the patient, did not become infected. A fourth diagnosis of Ebola infection in the United States occurred later in October when a doctor who had returned to New York from treating patients in Guinea tested positive for Ebola virus. He was hospitalized and has recovered and is free of the virus. His contacts completed the 21-day follow-up period without becoming infected.
At the end of 2014, the toll of reported cases stood at approximately 20,200, of whom more than 7,900 died. Actual numbers are thought to be higher. Nearly all of the deaths occurred in Liberia, Sierra Leone, and Guinea. There was one death in the United States, six in Mali, and eight in Nigeria. Until December, the highest numbers of cases and deaths had occurred in Liberia, but towards the end of 2014 the number of new cases surged in Sierra Leone surpassing the count in Liberia. Sierra Leone remains the country with the most confirmed cases of EVD, although the death toll is highest in Liberia.
Progress became apparent during the early months of 2015 when overall numbers of new cases declined. Towards the end of the year, the outbreak was declared over in Liberia in September, in Sierra Leone in November, and in Guinea in December after each of these countries completed a period of 42 days, double the maximum incubation time, in which no new confirmed cases were reported.
The WHO declared an end to the international public health emergency in West Africa at the end of March 2016. By this time, an overall total of more than 28,600 cases and 11,300 deaths had occurred as a result of this Ebola virus outbreak.
The 2018 Outbreaks in the Democratic Republic of the Congo
The first outbreak of Ebola virus in the Democratic Republic of the Congo of 2018 was reported in early May after two cases caused by the Ebola Zaire virus were confirmed in laboratory tests. This was the ninth EVD outbreak in the DRC in the last four decades (the prior one occurred in May 2017). The outbreak was declared ended by the WHO in July after contacts of confirmed cases who had been vaccinated did not display Ebola virus symptoms within 42 days (double the maximum incubation period for infection). In total, there were 54 confirmed or probable cases, including 32 deaths, as a result of this outbreak, which was confined to regions within the northwestern part of the country. The four cases in the large urban center of Mbandaka, a major transportation hub, had caused the greatest concern.
The short duration of the first 2018 outbreak appeared to be due to benefits from the scientific knowledge gained during the 2014 outbreak in West Africa and the results of a vaccination trial conducted in Guinea during 2015. Once the 2018 outbreak was reported, a wide partnership of governmental and health agencies worked quickly to curtail it. Using the rVSV-ZEBOV vaccine (developed by Merck) - which is not yet licensed nor formally approved - but was shown to be safe and effective during the vaccine trial in Guinea, a ring vaccination campaign was undertaken in which the contacts of confirmed cases, and their contacts, as well as healthcare workers and others with potential exposure to the virus were given the experimental vaccine. More than 3000 people were vaccinated.
The respite was short-lived, however, as on August 1, a little more than a week later, another outbreak - the tenth in the DRC - was declared. The new cluster of cases was reported in the North Kivu Province in the northeastern part of the country, a remote, conflict-plagued region that shares porous borders with Uganda and Rwanda and which hosts over a million displaced persons. These conditions have made it much more difficult to curtail the spread of the virus.
As of June 1 2019, a total of 1994 EVD cases in two neighboring northeastern provinces (North Kivu and Ituri) have been reported in this ongoing outbreak according to the World Health Organization. Of these cases, 1339 people have died (although the true number of cases and deaths is thought to be higher). This now ranks as the second largest Ebola epidemic ever (the 2014 outbreak in West Africa was the largest).
In spite of the use of proven control measures, such as ring vaccination (over 120,000 people have been vaccinated so far), and the availability of preventive and therapeutic tools, containment of the virus has been hindered by the geographical challenges, security hazards, distrust of authorities, and a lack of understanding about the disease. Efforts to control the outbreak were further challenged by attacks on two Ebola treatment centers in late February. The risk of continued national and regional transmission remains very high.
The Problem
Ebola virus is a class A bioterrorism agent, known to cause highly lethal hemorrhagic fever. The mortality rate can be as high as 90 percent. Because the Ebola virus is so hazardous, it is classified as a biosafety level 4 agent - the level assigned to the most dangerous agents known. Research using Ebola viruses requires facilities with the utmost levels of containment, strict controls on access, and highly trained personnel.
In addition to being classified as a potential bioterrorism agent, the risk of natural outbreaks and the further emergence of Ebola virus is a serious concern. As the human population grows, human contact with bats or Ebola-infected non-human primates increases, as does human to human spread particularly in the age of air travel. The 2014 Ebola virus disease outbreak in West Africa clearly illustrates this risk.
The latest outbreak in the Democratic Republic of the Congo, in the latter half of 2018, highlights the complex challenges of curtailing the spread of the virus in regions that are unstable and geographically remote and where there are high levels of misinformation and mistrust of authorities.
There is still no cure for Ebola virus disease and no established drug therapy to treat Ebola infection. There is no approved vaccine that can protect humans against Ebola, although an unlicensed vaccine has been shown to be effective. As is the case for many other viral diseases, such as Zika virus, Ebola was considered a neglected disease because until 2014 the total number of infections was low, so there was little investment in anti-viral research. Scientists lacked sufficient diagnostic tools to rapidly identify Ebola infections. Scientists still need a more thorough understanding about how the virus is transmitted and how it causes disease.
Ebola is a threat not only to humans but also to our closest living relatives - the great apes. In addition to threats due to poaching and habitat loss, chimpanzees and gorillas are susceptible to infection by Ebola virus, which can kill over 90% of infected animals. Past Ebola infections have wiped out about a third of the gorillas in protected areas, and the western lowland gorilla populations have been decimated by Ebola to such an extent that they are now considered "critically endangered".
2014 Outbreak
The 2014 Ebola outbreak was unprecedented for several reasons. First, it occurred in a region of Africa in which Ebola had never before been detected. This made it difficult for healthcare workers to swiftly identify Ebola as the cause of infection, whose early symptoms are similar to other diseases in the region. Second, unlike previous episodes which were confined largely to remote areas, this outbreak began near the borders of three countries - Guinea, Liberia, and Sierra Leone - where there is a lot of travel, and it spread rapidly not only to rural regions as in previous outbreaks, but also to densely populated areas. This resulted in an outbreak that involved multiple regions in the three hardest hit countries. Additionally, it was the first time that Ebola was carried by air travel from one country to another. Further, the outbreak occurred in countries with weak healthcare infrastructure and a population that is distrustful of government and healthcare workers. Because it encompassed a much wider geographic area and denser population areas than previous outbreaks, containment was vastly more difficult and complex.
It was an immense challenge to control the outbreak in this impoverished part of the world, lacking many basic and essential medical supplies. Workers faced the daunting task of identifying and quarantining large numbers of infected individuals and their contacts and providing medical care to patients - without sufficient numbers of health workers, personal protective equipment, adequate facilities, or sufficient numbers of hospital beds. Many infected individuals initially were turned away from health facilities and sent home, where they were more likely to infect others, due to lack of space in hospitals. Workers also needed to educate a fearful and mistrustful population about the dangers of Ebola and the proper procedures needed to minimize further infections, including safe burial procedures.
Health care workers themselves were at high risk of infection; more than 870 became infected and at least 500 died. Even outside of West Africa, there were several infections of health care workers - one in Spain and two in Dallas - within hospital settings in developed countries that employed rigorous infection control in workers wearing protective gear while treating Ebola infected patients.
The Ebola outbreak had a significant social and economic effect on the impacted regions in West Africa. Travel restrictions were put in place, schools were closed, and general panic and misinformation arose in some areas. Fear, and loss of health care workers and even attacks on these workers, led to the collapse of health care systems in some affected areas, which resulted in deaths due to other diseases that normally would be treatable. The outbreak also created orphans, which were often unwanted by extended family members due to fear that the child could spread the disease.
In the United States, the arrival of a person traveling from Liberia to Dallas and his subsequent diagnosis of Ebola infection, as well as the diagnosis of EVD in a doctor returning to New York after treating Ebola patients in West Africa also caused some panic in the United States. This led to the institution of some mandatory quarantines and travel restrictions of persons returning from Ebola-affected areas. It also created a stigma associated with recovered patients or those who have treated Ebola patients. Some of the policies were medically unnecessarily restrictive and may have discouraged volunteers from traveling to West Africa to treat patients at the source of the outbreak.
The lack of approved drugs and vaccines highlights the general problem of inadequate funding for diseases that have previously occurred only in remote areas and afflicted small numbers of people. A major problem during the height of the 2014 outbreak was that the experimental drugs and vaccines were available in extremely limited quantities and they had not undergone extensive prior testing in humans. Production was scaled up, but they were not widely available until late in the outbreak. The availability of limited quantities of drugs and vaccines that have not been fully tested raises ethical concerns regarding the administration of unapproved drugs and determining which patients or workers should receive the drugs when there is a scarce supply.
A serious concern during any outbreak is the possibility that the virus could mutate to a form that is more virulent or contagious or becomes transmissible through the air where it could infect larger numbers of people. The reason for this concern is that when viruses pass through a large number of people, the number of mutations increases. Although some changes to the Ebola virus did occur, the strain that circulated during the 2014 Ebola outbreak is very similar to the strain initially discovered in 1976, and the changes did not appear to affect the ability of the virus to cause disease.
In order to prevent another large Ebola virus outbreak, it is critical to maintain a high level of vigilance, so that any new cluster of infections can be swiftly identified and contained, as well as continuing the development and testing of vaccines and drugs that can be used in future outbreaks of the Ebola virus.
The Research
One of the key steps in any virus infection occurs very early in an infection cycle. That is the step where a virus binds to and enters a cell in a susceptible host organism. Because viruses are too small to reproduce on their own, they must invade a host cell in order to multiply and produce more copies of themselves that can then go on to infect other organisms and continue the infection cycle.
Many viruses require a specific protein or other type of molecule on the surface of the host cell - called a receptor - which allows the virus to pass into a cell of a host organism. If an organism or cell type does not possess this particular receptor, the virus is unable to infect that organism or cell type. Knowing what this receptor is for any particular virus is a crucial piece of information for scientists, because it tells them which organisms or cell types are susceptible to infection by a certain virus. It is known that in humans, the Ebola virus appears to infect many different cell types. Ebola is also thought to have a broad host range, since it is capable of infecting diverse mammalian species, including primates, rodents, and bats. This knowledge can be used to design therapies that may be able to prevent a virus from entering into a cell and initiating an infection.
Dr. Richard Sutton, while in the Department of Molecular Virology and Microbiology at Baylor College of Medicine, sought to identify the Ebola virus receptor. Based on evidence from other scientists that suggested that members of a group of proteins named the Tyro3 family might mediate entry of Ebola virus into cells, Dr. Sutton’s group tested what would happen if they reduced the levels of the Tyro3 proteins in cells. They reasoned that if these proteins were necessary for entry into cells, reduction of their levels should diminish infection by Ebola. However, they observed little effect on Ebola virus infection when they reduced levels of expression of all three Tyro3 family genes. They therefore concluded that it is unlikely that this family of proteins is the entry factor for Ebola virus.
In addition, Dr. Peter Hotez, professor of Molecular Virology and Microbiology, and Pediatrics, and founding dean of the National School of Tropical Medicine at Baylor College of Medicine provided his expertise on the Ebola virus during the 2014 Ebola outbreak and gave interviews to numerous media outlets. He was named to the Texas Task Force on Infectious Disease Preparedness and Response created in 2014.
Glossary
Learn more about some of the technical terms found on our glossary of terms page.
View an Ebola Presentation
2014 Ebola Virus Outbreak (ppt)








 Credit
Credit