Researchers identify an Achilles’ heel in neuroblastoma
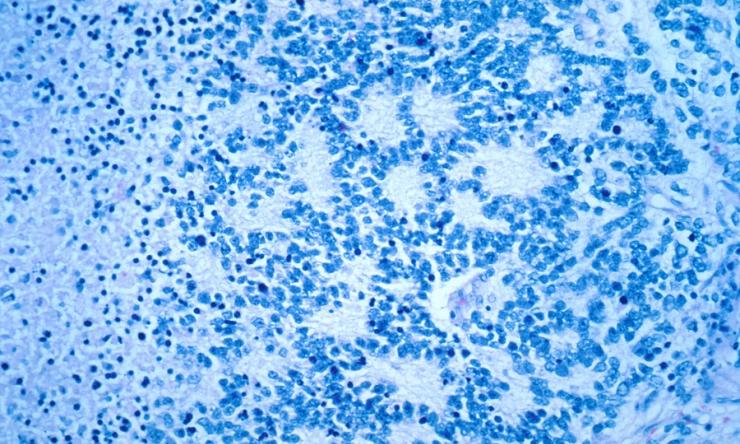
Neuroblastoma, a childhood cancer that develops from neural cells on the adrenal glands, accounts for 15% of childhood cancer deaths. Almost half of children with high-risk neuroblastoma harbor extra copies of the gene MYCN (MYCN amplified), the primary driver of neuroblastoma and its resistance to therapy.
“Treating neuroblastoma by directly targeting MYCN has been challenging,” said Dr. Eveline Barbieri, corresponding author of a recent study on neuroblastoma published in the journal Nature Communications and assistant professor of pediatrics – hematology and oncology at Baylor College of Medicine and Texas Children’s Hospital. “In this study we investigated new strategies to improve the survival of children with MYCN amplified neuroblastoma by looking into metabolic vulnerabilities that we could exploit to overturn these tumors’ resistance to therapy.”
Barbieri and her colleagues used an unbiased, metabolomics analysis to compare the metabolic profiles of MYCN-amplified neuroblastomas to the profiles of non MYCN-amplified neuroblastomas. The results of their innovative approach showed that there were important differences between tumor cell utilization of specific nutrients for tumor growth in these two tumor groups.
“We found that MYCN amplification rewires a tumor’s lipid metabolism in a way that promotes the use and biosynthesis of fatty acids, a type of lipid cells can use as a source of energy,” Barbieri said. “Cells with extra copies of MYCN depend highly on fatty acids for their survival. We confirmed this both in MYCN-amplified cell lines and in MYCN- amplified patient tumor samples.”
Barbieri and her colleagues hypothesized that MYCN reroutes lipid metabolism so that fatty acids are readily available to cancer cells, thereby promoting tumor cell growth.
Looking into the mechanism
“When we investigated what prompted MYCN-amplified neuroblastomas to rely on fatty acids to grow, we discovered that MYCN directly upregulates or enhances the production of fatty acid transport protein 2 (FATP2), a molecule that mediates cellular uptake of fatty acids,” Barbieri said. “We then asked, what would happen if we interfered with FATP2 function in MYCN-amplified neuroblastomas?”
When the researchers neutralized FATP2 activity, either by knocking down the gene or by blocking FATP2 action with a small-molecule inhibitor, they reduced the growth of MYCN-amplified tumors.
“We observed that when we blocked the import of fatty acids into the cancer cells, and there was a reduction in tumor cell growth,” Barbieri said. “The interesting part is that inhibiting or blocking FATP2 had no effect on normal cells or tumors without MYCN-amplification. This seems to be a selective metabolic vulnerability of MYCN-amplified tumors. They uniquely use this transporter to feed on fatty acids to grow.”
There are other MYCN-amplified pediatric and adult tumors.
“This approach may be applicable to many human cancers that utilize MYC for oncogenesis (about 50% of cancers overall) and provide new insight into the regulation of energy metabolism in cancer progression,” Barbieri said.
These finding suggest that therapeutic interventions that interfere with FATP2 activity can potentially selectively block fatty acid uptake in MYCN-amplified tumors, stopping or reducing tumor growth and making them more sensitive to conventional chemotherapy.
“More work is needed before this approach can be employed in the clinical setting,” Barbieri said. “But this study suggests that strategies to interfere with a tumor’s nutritional dependence on fatty acids is a promising therapeutic strategy worthy of further investigation.”
Other contributors to this work include first author Ling Tao and Mahmoud A. Mohammad, Giorgio Milazzo, Myrthala Moreno-Smith, Tajhal D. Patel, Barry Zorman, Andrew Badachhape, Blanca E. Hernandez, Amber B. Wolf, Zihua Zeng, Jennifer H. Foster, Sara Aloisi, Pavel Sumazin, Youli Zu, John Hicks, Ketan B. Ghaghada, Nagireddy Putluri, Giovanni Perini and Cristian Coarfa. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Dan L Duncan Comprehensive Cancer Center, National Research Center-Cairo, University of Bologna, Texas Children’s Hospital and Houston Methodist Hospital.
This study was supported by the Kate Amato Foundation and the Department of Defense (W81XWH-19-1-0556). See the publication for a full list of funding for each study author.