PLAIN RADIOGRAPHIC DIAGNOSIS OF CONGENITAL HEART DISEASE |
Contents | Previous Condition | Next Condition
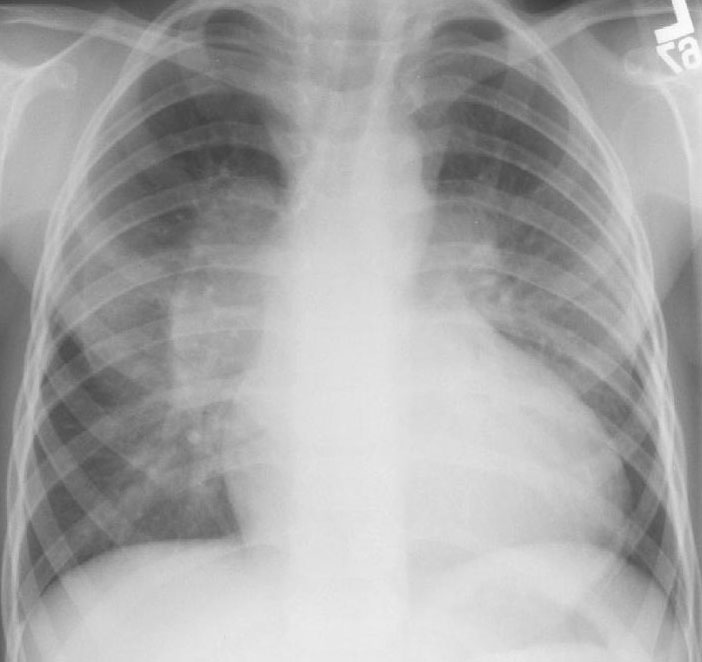
A. The left and right pulmonary arteries are markedly prominent with slightly reduced peripheral vascular markings.
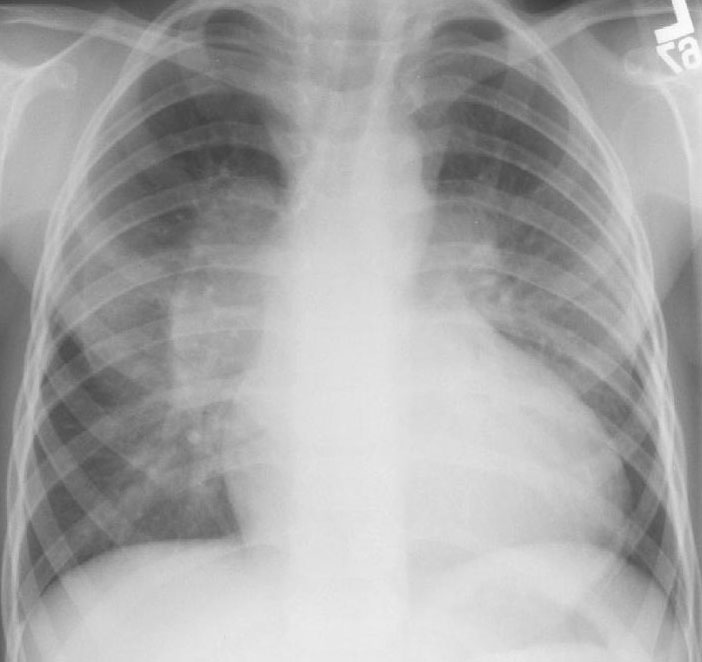
Congenital absence of the pulmonary valve leaflets in association with tetralogy of Fallot was first reported by Crampton in 1830. Between 2-6% of patients with tetralogy have co-existent absent pulmonary valve syndrome.
This is characterized by either a complete absence of the pulmonary valve leaflets or a rudimentary rim of tissue, typically in association with stenosis of the pulmonary annulus and infundibulum. The most characteristic feature of the syndrome however is aneurysmal dilation of the main pulmonary artery and the branch pulmonary arteries. The aneurysmal pulmonary arteries compress the bronchi and create a ball-like effect with resultant significant airway problems.
Associations: Commonly there is an associated defect including ASD, DORV, hypoplastic right ventricle, tricuspid atresia, transposition of the great arteries, Uhl’s anomaly, coarctation or subaortic stenosis.
All patients must be screened for 22q11 deletion and associated DiGeorge syndrome.
Presentation: Newborns may present with cyanosis secondary to elevated pulmonary vascular resistance and reduced right ventricle compliance. Congestive cardiac failure secondary to left to right shunting through a VSD although this is often prevented by the right ventricular outflow tract obstruction. Typically recurrent chest infections are the presenting feature secondary to air-trapping from the bronchial and bronchiolar compression, resulting from the aneurysmal pulmonary vessels. Physical examination is characteristic for a high pitched systolic ejection murmur and a low pitched diastolic descrescendo murmur heard maximally in the third left intercostal space.
Treatment: There is little consensus to the optimum surgical treatment. Plication of the pulmonary arteries may provide temporary respite from intercurrent respiratory illness, although the natural history is for the development of recurrent aneurysmal dilation and respiratory morbidity. Whether a two-stage approach with initial pulmonary artery banding to reduce pulmonary arterial circulation followed by intracardiac repair and debanding is preferable remains unknown. There is also debate as to whether placement of a valve in the pulmonary position may improve prognosis. Generally the earlier surgical plication is required the worse the prognosis.