Patient #14, a 46 year old white female, presented with complaints of rapidly progressive headache, neck stiffness, tinnitus, hearing impairment, eye pain, and loss of vision in both eyes.
The patient was well until three weeks prior to admission when she developed "flu-like" symptoms with an upper respiratory infection, low-grade fever, and cough. She was seen by her primary physician who prescribed antibiotics for two days.
One week later, she complained of bilateral frontal headaches which were initially mild but worsened over the ensuing days. The headaches were exacerbated on lying down and were worse in the afternoon. At about the same time, she noted blurring and distortion of vision (she saw the floor as "bumpy"). She was prescribed new eye glasses, but her vision continued to deteriorate.
Subsequently, she noted that she did not hear well during conversations and phone calls, and complained of "ringing" in the ears (worse on the right side). She also complained of neck stiffness which was aggravated on leaning forward. She had difficulty with concentration and memory, requiring her husband to "check her calculations" at work.
Several days prior to presentation, she complained of increasing headaches and neck stiffness, trouble sleeping, redness in both eyes, and pressure-like eye pain partially relieved on sitting up. She presented to the Emergency Room with neck stiffness, severe headache/eye pain, injected and swollen eyes, and markedly blurred vision.
Past Medical History: The patient did not smoke and consumed alcohol occasionally. She is married with one daughter and works with her husband in business. Her history was negative for exposure to chemicals, drug abuse, and risk factors for sexually transmitted diseases. She had a hysterectomy fourteen years previously and deep venous thrombosis following trauma three years ago, for which she took coumadin for six months.
She had a prior history of an irregular heart beat which required medication. She had no known allergies, no history of ocular surgery or trauma, previous eye disease, photosensitivity, or skin changes including rashes, acne, or vitiligo. She also had a negative history for alopecia, poliosis, joint disease, mouth ulcers, abdominal complaints, diarrhea, constipation, urinary symptoms, hematuria, easy bruising, or repeated infections.
General: Middle aged lady appearing stated age, but in obvious discomfort.
Vital Signs: BP=184/106, HR=90, T=97.8, RR=20.
HEENT: Mild discomfort with neck flexion. Diffusely injected conjunctivae and periorbital swelling bilaterally. No lymphadenopathy, carotid bruit, or malar rash. Nose and mouth mucosa clear. Eardrums had normal light reflection bilaterally.
Chest: Clear to auscultation bilaterally.
Cardiovascular: Normal S1 and S2 with regular rate and rhythm, no murmurs.
Abdomen: Soft, normal bowel sounds. No hepatosplenomegaly or tenderness.
Extremities: No edema, cyanosis, clubbing, joint swelling, redness, or tenderness. Normal range of motion.
Skin: No lesions, acne, or ulcers.
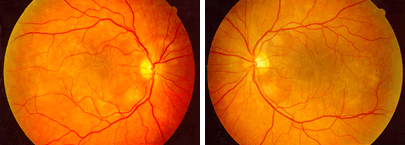
Ophthalmoscopic Examination: OD and OS, respectively
Mental Status: Awake, fully oriented and cooperative. Language parameters normal, immediate and delayed memory intact. She could not subtract 7 from 100, could spell "world" correctly, but could not spell the word backwards. Remainder of mini-mental exam was normal.
Cranial Nerves:
Cranial Nerves | Findings |
|---|---|
| I | Not tested |
| II | Pupils 4mm, reactive to light bilaterally. Best corrected visual acuity, 20/300 OD and 20/70 OS. Visual fields intact to confrontation. |
| III / IV / VI | Extraocular movements intact. |
| V | Normal to light touch, pinprick, temperature, and proprioception. Normal masseter, temporalis, and pterygoids motor strength. |
| VII | Symmetrical face and smile. Elevates eyebrows bilaterally. |
| VIII | Intact to finger rubbing bilaterally. No lateralization on Weber. |
| IX / X | Midline elevation of the uvula. Intact gag bilaterally. |
| XI | Normal sternocleidomastoid and trapezius muscles bilaterally. |
| XII | Midline tongue with normal bulk and tone. |
Motor: Normal bulk and tone. Normal muscle strength throughout (5/5).
Reflexes: 3+ throughout, with spread. Positive jaw jerk, bilateral Hoffman's sign, and bilateral Babinski.
Sensation: Normal light touch, pinprick, and temperature. Decreased vibration in the lower extremities and, to a lesser extent, in the upper extremities to the elbows bilaterally. Slightly decreased proprioception in the toes and fingers.
Coordination: Intact finger-to-nose, heel-to-shin, and rapid alternating movements.
Gait: Normal stance and gait, arm swing, and toe/heel walking. Slight swaying in Romberg position with the eyes closed, without loss of balance. Mild difficulty with tandem walk.
Email comments: