PLAIN RADIOGRAPHIC DIAGNOSIS OF CONGENITAL HEART DISEASE |
Contents | Previous Condition | Next Condition
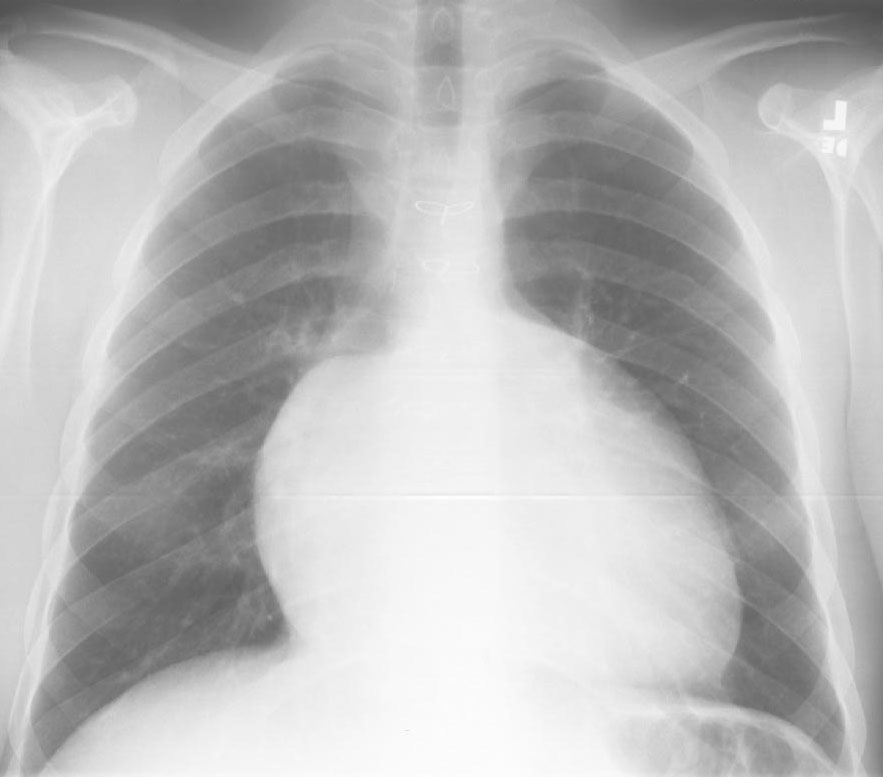
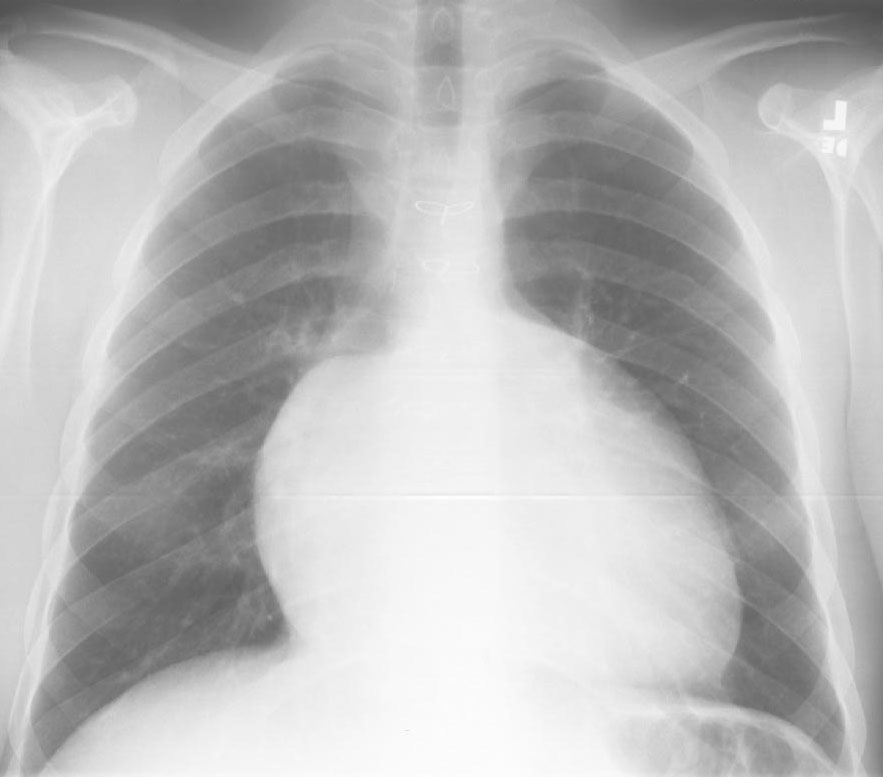
A. There is marked cardiomegaly with right atrial dilation and diminished pulmonary arterial markings.
Wilhelm Ebstein decribed this lesion in a 19 year old Polish worker on autopsy in 1866. Ebstein’s anomaly is characterized by displacement of the posterior and septal leaflets of the tricuspid valve towards the right ventricular apex. The commissure between the two is the point of maximal displacement and is at the posterior border of the ventricular septum. The anterior leaflet is not displaced and is sail-like and occasionally fenestrated. The right atrium is usually dilated and the tricuspid valve annulus is enlarged. The inferior vena cava valve is markedly prominent. The atrialized portion of the right ventricle has a thiner wall tha the functional right ventricle. In patients with congenitally corrected transposition of the great arteries there may be co-existent Ebstein’s anomaly. In the majority of cases there is an atrial septal defect (90%). Pulmonary stenosis or atresia occurs in a small percentage and VSD is rarely found.
Ebstein’s occurs in approximately 1 per 210,000 births and constitutes less than 1% of all congenital heart lesions. There is an equal sex distribution and lithium has been implicated as a causative factor.
Physical findings: This depends on the stage of presentation of the disease. In infants with right to left shunt there may be a cyanosis which is accompanied by clubbing in older children. The first heart sound is widely split secondary to increased excursion of the anterior leaflet and delayed closure of the tricuspid valve. The second heart sound is also widely and persistently split owing to delayed closure of the pulmonary valve. A pansystolic murmur is heard at the left lower sternal edge and epigastrium secondary to tricuspid regurgitation. There may also be low intensity diastolic murmurs secondary to anterograde flow across the tricuspid valve. These murmurs are increased on inspiration secondary to decrease in intrathoracic pressure and increased inflow across the tricuspid valve.
CXR: The right atrium is often grossly enlarged and there is impressive diminution of pulmonary arterial markings secondary to right to left shunting through the atrial septal defect. Often the heart is massively enlarged secondary to the right atrial dilation and may take up most of the chest, the so-called "wall to wall" heart.
ECG: There is often first degree AV block (1/3 patients), right atrial enlargement (1/3-1/4 patients), and right axis deviation, right bundle branch block, but rarely right ventricular hypertrophy. Between 4-26% of patients have Wolff Parkinson White which is nearly always type B. Arrthymias including supraventricular tachycardia and ventricular tachyarrthymias amy occur. Simultaneous radiofrequency ablation of accessory pathways may be performed either before or at the same time as surgical attention (replacement or annuloplasty) to the tricuspid valve.
ECHO: The features of Ebsteins’s including displacement of the posterior and septal leaflets of the tricuspid valve, enlargement of the right atrium and atrialization of the right ventricle can be assessed. On M-mode there is increased amplitude and velocity of the anterior leaflet tricuspid leaflet, paradoxic septal motion, and delayed closure of the anterior tricuspid valve leaflet. Delayed closure of the tricuspid valve more than 50 milliseconds after the mitral valve may indicate the presence of Ebstein’s anomaly although this may occur in right bundle branch block. Other features include excessive elongation of the anterior leaflet of the tricuspid valve and leaflet tethering to the underlying myocardium of any of the leafletsor rarely absence of the septal or posterior tricuspid leaflets.