
PLAIN RADIOGRAPHIC DIAGNOSIS OF CONGENITAL HEART DISEASE |
Contents | Previous Condition | Next Condition
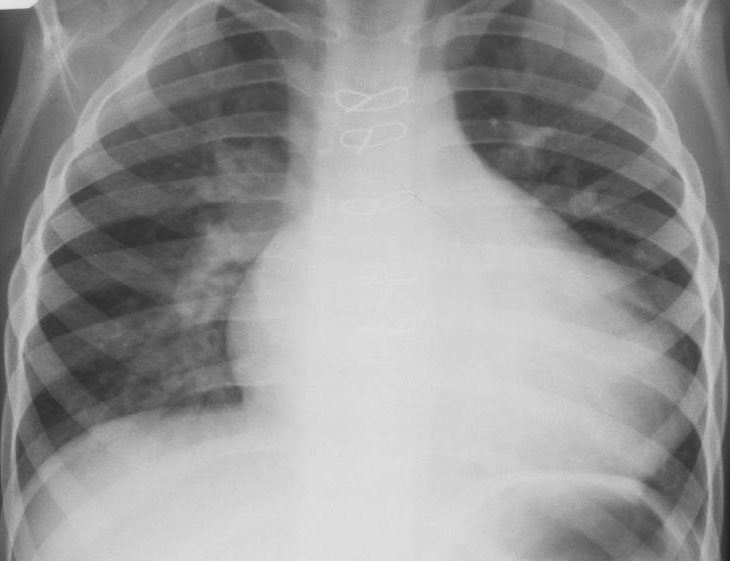
A. PA chest radiograph demonstrates cardiomegaly, the pulmonary outflow tract is convex and the pulmonary arterial markings are increased.

B. Right anterior oblique view demonstrates posterior displacement of the esophagus indicating left atrial dilation in addition to bi-ventricular enlargement. Hilar dance was noted at flouroscopy.

A. PA chest radiograph demonstrates moderate cardiomegaly with the left ventricular apex extending to the left chest wall. The pulmonary vascular markings are bilaterally symmetrically increased and the pulmonary outflow tract is convex. The patient has had a sternotomy.
A. PA chest radiograph demonstrates marked cardiomegaly with bilaterally increased pulmonary arterial markings. Air trapping is appreciable in the right middle lobe.
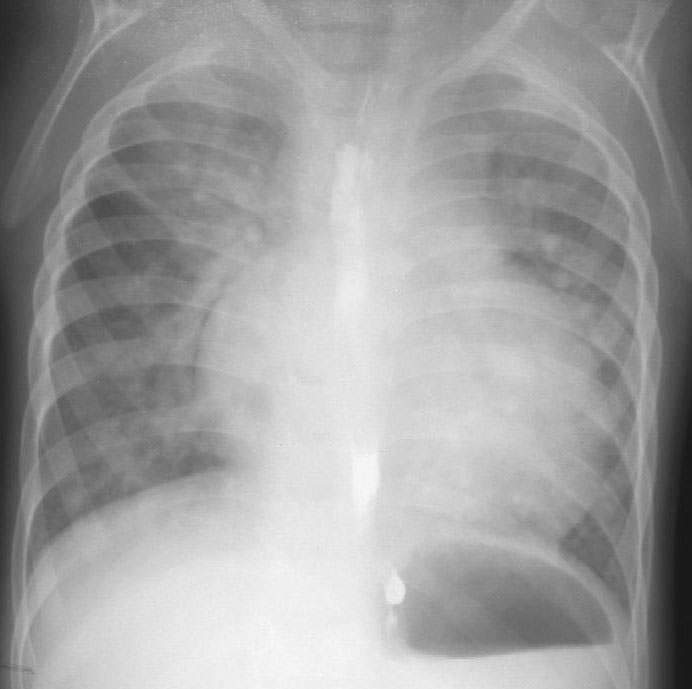
B. Right anterior oblique film and barium swallow demonstrates left atrial compression of the esophagus confirming left atrial dilation.

VSDs represent the commonest form of congenital heart disease. This lesion was first described by Roger in 1879 giving his name to small asymptomatic ventricular septal defects "maladie de Roger". With the advent of cardiac catheterization and real time 2D echocardiography a classification system of VSDs evolved.
Incidence: This lesion accounts for approximately 20% of patient visits to the cardiology clinic with a reported incidence of 1.5-2 per 1000 live births.
Classification:
Perimembranous inlet may be associated with malaignment of the ventricular septum with the atrial septum, and perimembranous outlet defects with malalignment of the ventricular and infundibular septum (often in association with conotruncal defects including tetralogy of Fallot and truncus arteriosus).
Embryology: Formation of the interventricular septum occurs by fusion of endocardial cushion tissue, from the conus septum, with the superior portion of the muscular septum and a portion of the right superior endocardial cushion. Defects involving the outlet septum are thought to arise from failure of fusion of components of the conus septum. Defects of the inlet septum from failure of fusion of the right superior endocardial cushion tissue with the muscular septum. Muscular defects (particularly trabecular) are probably secondary to excessive excavation of septum during ventricular growth or inadequate merging of the medial walls of the ventricles.